Once we consider utilization administration (e.g., prior authorizations, step edits), we frequently suppose payers solely use these for larger value branded merchandise together with biologics. Generic medication ought to have low value sharing and restricted utilization administration. One query, nonetheless, is whether or not payers’ utilization administration practices for biosimilars mirror these of biologic merchandise, or small-molecule generics, or someplace in between.
A paper by Yu et al. (2023) goals to reply this query. The authors used information from the Tufts Medical Middle Specialty Drug Proof and Protection (SPEC) database masking 19 commercially-available biosimilars akin to 7 reference merchandise. These merchandise had been used for 28 distinctive indications. The authors discover that:
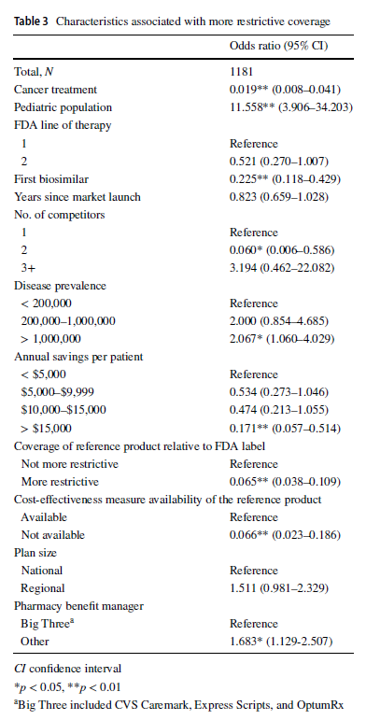
In contrast with reference merchandise, well being plans imposed protection exclusions or step remedy restrictions on biosimilars in 229 (19.4%) selections. Plans had been extra prone to prohibit biosimilar protection for the pediatric inhabitants (odds ratio [OR] 11.558, 95% confidence interval [CI] 3.906–34.203), in illnesses with US prevalence larger than 1,000,000 (OR 2.067, 95% CI 1.060–4.029), and if the plan didn’t contract with one of many three main pharmacy profit managers (OR 1.683, 95% CI 1.129–2.507). In contrast with the reference product, plans had been much less prone to impose restrictions on the biosimilar–indication pairs if the biosimilar was indicated for most cancers remedies (OR 0.019, 95% CI 0.008–0.041), if the product was the primary biosimilar (OR 0.225, 95% CI 0.118–0.429), if the biosimilar had two opponents (reference product included; OR 0.060, 95% CI 0.006–0.586), if the biosimilar may generate annual listing worth financial savings of greater than $15,000 per affected person (OR 0.171, 95% CI 0.057–0.514), if the biosimilar’s reference product was restricted by the plan (OR 0.065, 95% CI 0.038–0.109), or if a cost-effectiveness measure was not accessible (OR 0.066, 95% CI 0.023–0.186).
One attention-grabbing discovering was that enormous PBMs truly had much less restrictive insurance policies over biosimilars. Why?
… it has been posited that the bargaining energy of bigger PBMs could also be so vital that biosimilar producers could typically increase listing costs, and therefore rebates, to acquire a spot on the formularies of huge PBMs. This would go away smaller PBMs with larger listing costs however
smaller rebates attributable to their comparatively smaller bargaining energy, through which case the biosimilars carry much less worth to them.
You’ll be able to learn the total paper right here.